Cardiovascular diseases remain the leading cause of death worldwide.
Despite preventive efforts—such as controlling LDL cholesterol, blood pressure, and glucose levels—many individuals still suffer heart attacks or strokes even with apparently “normal” values.
This phenomenon is known as residual cardiovascular risk, and it accounts for up to 60–70% of cases. A study published in the American Heart Journal in 2009, based on more than 130,000 patients hospitalized for coronary artery disease, showed that over 50% had optimal LDL cholesterol levels at the time of admission. This finding highlights that LDL cholesterol alone is not a sufficient indicator of cardiovascular risk (1).
Figure 1: Histogram of LDL levels at admission in 10 mg/dL increments.
Biosfer Teslab was founded with the mission of transforming the way we evaluate and understand lipid metabolism and cardiovascular risk, using innovative tools based on nuclear magnetic resonance (NMR) technology.
This mission took shape with the development of the Liposcale® test, which enables a much more detailed and functional analysis of the lipid profile. Unlike traditional tests that measure only total cholesterol, LDL, or HDL, Liposcale® goes further:
It analyzes the distribution of lipoprotein particles based on their size and concentration, helping to identify subtypes of dyslipidemia that may go undetected with a conventional lipid profile.
It assesses the triglyceride content transported in each type of lipoprotein, which is key in studying atherogenic dyslipidemia and in patients with metabolic syndrome.
It detects altered lipid profiles that may be missed in standard analyses, such as a high number of small, dense LDL particles, which are highly atherogenic.
It offers a more personalized approach to cardiovascular prevention and treatment, allowing therapeutic strategies to be tailored to each patient’s true lipoprotein profile, not just their total cholesterol.
Thanks to this technology, it is now possible to identify true risk profiles in patients who, under conventional criteria, might appear to be at low risk.
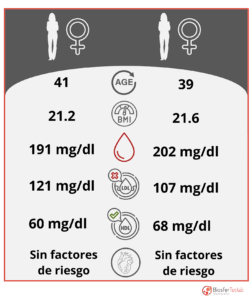 We present the case of two women of similar age (41 and 39 years), with no known risk factors and a normal body mass index (21.2 and 21.6 kg/m², respectively). Both have appropriate levels of total cholesterol, LDL, and HDL. At first glance, their cardiovascular profiles appear healthy.
We present the case of two women of similar age (41 and 39 years), with no known risk factors and a normal body mass index (21.2 and 21.6 kg/m², respectively). Both have appropriate levels of total cholesterol, LDL, and HDL. At first glance, their cardiovascular profiles appear healthy.
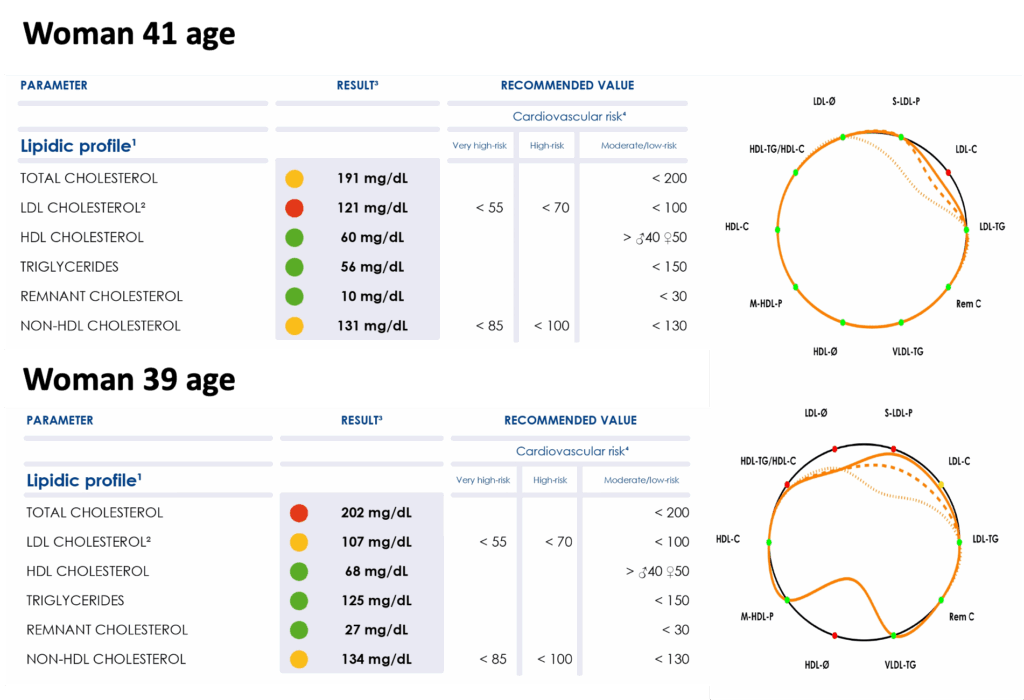
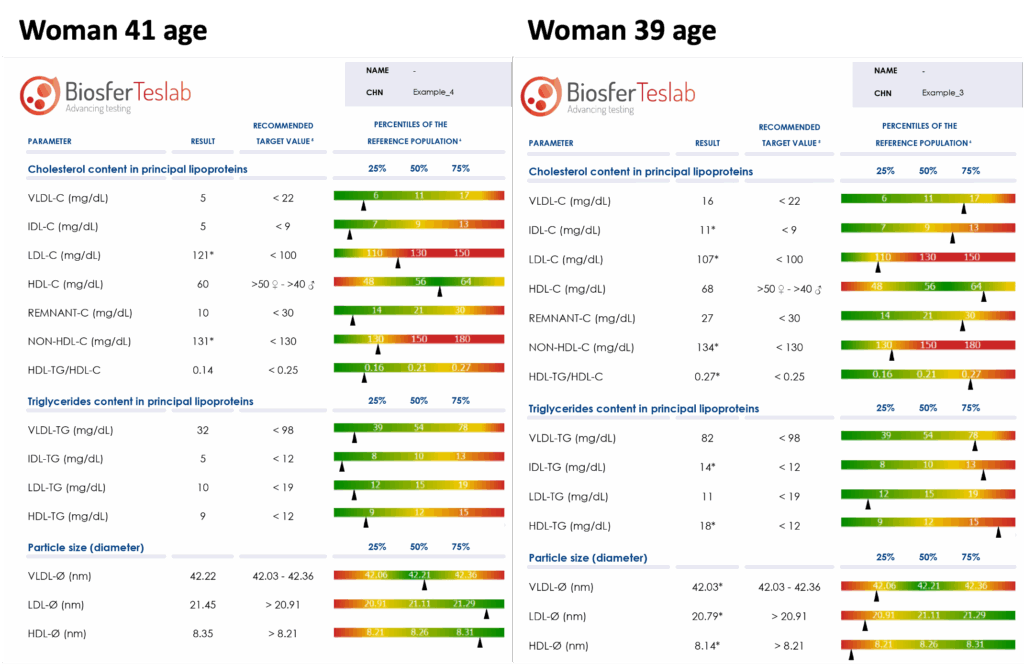
However, when both women underwent evaluation using the Liposcale® test, the results told a different story. Although their standard lipid profiles (Figure 3, left) appear quite similar, a more detailed analysis of their lipid profiles (Figure 3, right) reveals significant differences. Interestingly, the woman with the lower LDL cholesterol levels shows more pronounced alterations in her lipoprotein profile, which is clearly reflected in her lipid signature.
A closer look at a portion of the comprehensive lipid panel provided by the Liposcale® test (Figure 4) shows that, while both women present fairly similar values, one tends to fall within the green range, whereas the other displays more values in the yellow range. This suggests that, despite having seemingly normal values in conventional parameters, the latter has a more pro-atherogenic profile and therefore a higher cardiovascular risk, even in the absence of traditional risk factors. Moreover, the analysis of the mean particle size further supports this pattern, once again indicating a more pro-atherogenic profile in her case.
Thus, the use of the Liposcale® test for a detailed characterization of the lipoprotein profile allows for more accurate and valuable information in the assessment of cardiovascular risk. This approach goes beyond conventional parameters such as LDL cholesterol, HDL, or triglycerides, by analyzing key aspects like the number, size, and distribution of lipoprotein particles.
In this specific clinical case, although the standard lipid profile values were within normal ranges, the advanced analysis using Nuclear Magnetic Resonance (NMR) technology revealed relevant metabolic alterations that would not have been detected with traditional methods. This result highlights the presence of residual cardiovascular risk that, if not identified, could have gone unnoticed in routine clinical practice.
The findings obtained through the Liposcale® test reinforce the importance of adopting more comprehensive and sensitive diagnostic tools in the management of cardiovascular disease. Thanks to this detailed evaluation, it is possible to offer more accurate risk stratification, improve clinical decision-making, and move toward truly personalized medicine, where each patient receives analysis and follow-up tailored to their actual metabolic profile.
The Liposcale® test provides an advanced view of the lipid profile, essential for identifying residual risk that conventional blood tests may miss.
Get in touch with our scientific team to learn how to integrate this tool into your clinical practice or research projects:
Practical details: Biosfer Teslab Portfolio
Reference:
Sachdeva, A., Cannon, C. P., Deedwania, P. C., et al. (2009). Lipid levels in patients hospitalized with coronary artery disease: an analysis of 136,905 hospitalizations in Get With The Guidelines. American Heart Journal, 157(1), 111-117. https://doi.org/10.1016/j.ahj.2008.08.010