For decades, LDL cholesterol has been considered the main enemy in cardiovascular prevention. However, numerous studies — including the FOURIER-OLE trial — have shown that even patients with extremely low LDL-C levels continue to experience cardiovascular events.
This phenomenon is known as residual cardiovascular risk.
Among the contributing factors, triglycerides (TG) and triglyceride-rich lipoproteins (TRLs) stand out as key players. These particles, which include VLDL and their remnants, are highly atherogenic, and their excess reflects a global disturbance of lipid metabolism.
The study, published by Núria Amigó, Pol Torné, Liv T. Nordestgaard, Francesco Di Giacomo-Barbagallo, Carla Merino, Paolo Magni, Ana González-Lleó, Natalia Andreychuk, Alberico L. Catapano, Lluís Masana, and Daiana Ibarretxe, investigated how rising triglyceride levels modify the entire lipoprotein profile.
The research team used nuclear magnetic resonance (¹H-NMR) spectroscopy — via the Liposcale® method — in 822 patients with metabolic alterations followed at a specialized hospital lipid unit.
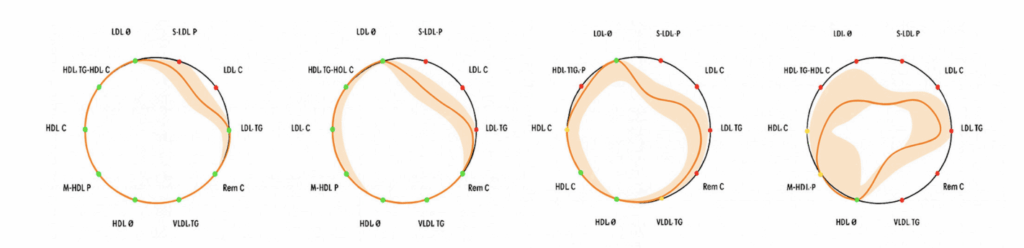
In addition, they developed an innovative visualization tool called the “Lipid Silhouette” (LS), a circular graphical representation summarizing ten key lipoprotein parameters, allowing clinicians to instantly visualize how higher TG levels distort the patient’s lipid balance.
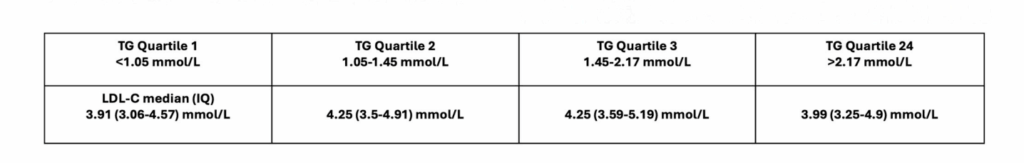
Participants were divided into triglyceride quartiles, from normal values (<1.05 mmol/L) to hypertriglyceridemia (>2.17 mmol/L). The results were striking:
Together, these changes define a global pro-atherogenic lipoprotein profile, clearly visible through the lipid silhouette, which progressively contracts as triglyceride levels rise.
Although obesity and type 2 diabetes often accompany hypertriglyceridemia, the study showed that lipoprotein disturbances persisted even in patients without these conditions, reinforcing that triglycerides are a direct determinant of metabolic imbalance.
Both men and women exhibited similar patterns of lipoprotein deterioration as TG concentrations increased.
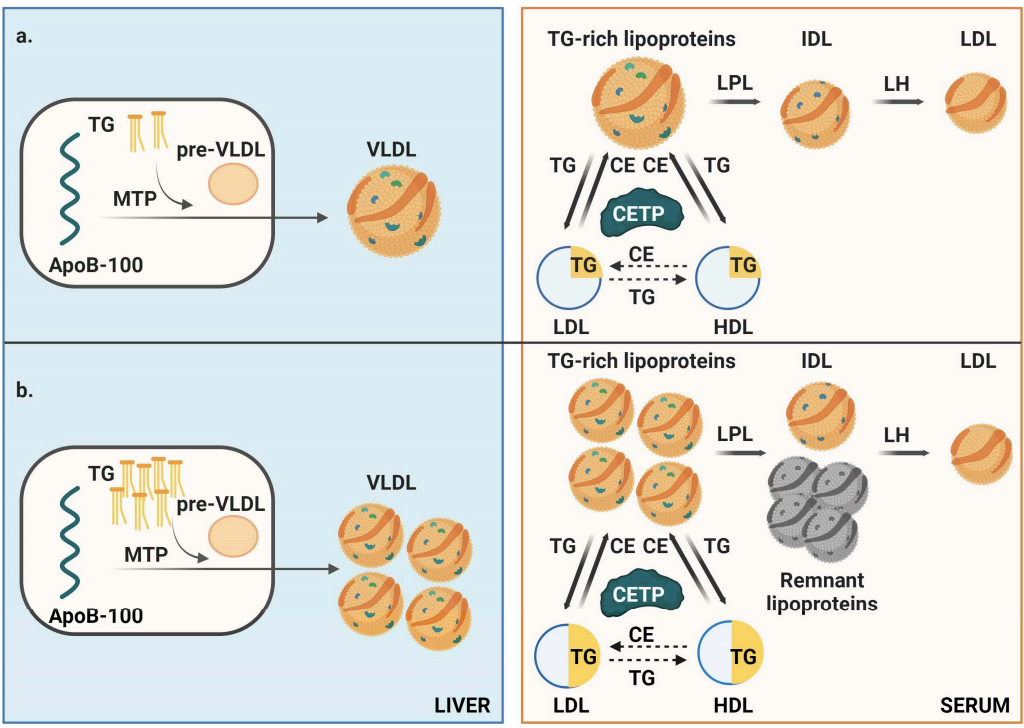
The authors propose a model in which hepatic triglyceride accumulation stimulates the overproduction of VLDL particles, increasing the total number of apoB-containing atherogenic lipoproteins.
In states of hypertriglyceridemia, the activity of lipoprotein lipase (LPL) becomes saturated, impairing TRL clearance and generating partially delipidated remnants with greater arterial retention.
Moreover, the cholesteryl ester transfer protein (CETP)–mediated lipid exchange becomes dysfunctional, producing small, dense, TG-enriched LDL and HDL particles with compromised structure and reduced protective function.
The authors emphasize that triglyceride control should be considered a key target in cardiovascular prevention — beyond LDL-C alone.
Highlighted strategies include:
Even moderate elevations in triglycerides can profoundly disrupt the entire lipoprotein spectrum. Therefore, advanced monitoring tools such as Liposcale® ¹H-NMR profiling can offer a comprehensive view of residual cardiovascular risk.
The study concludes that triglycerides are not merely a component of atherogenic dyslipidemia — they are a key driver of global lipoprotein derangement.
Advanced ¹H-NMR characterization enables early detection of these alterations and supports personalized therapeutic decisions.
Visualizing the “Lipid Silhouette” provides clinicians and patients with a clear, intuitive picture of lipid metabolism, helping guide more precise and effective cardiovascular prevention.
Read the full paper here https://www.mdpi.com/1422-0067/26/17/8284