In 2022, over 2.5 billion adults were overweight, of which more than 890 million were obese. This represents 43% of adults over 18 years old (43% of men and 44% of women), a significant increase from 25% in 1990. The situation among children and adolescents is also alarming: more than 390 million young people aged 5 to 19 were overweight in 2022, with prevalence rising from 8% in 1990 to 20% in 2022. This increase affects both boys and girls, with 19% of girls and 21% of boys being overweight.
Overweight and obesity result from an imbalance between caloric intake (diet) and caloric expenditure (physical activity). In many cases, obesity is multifactorial, influenced by an obesogenic environment, psychosocial factors, and genetics. In some patients, specific causes can be identified, such as medications, illnesses, physical inactivity, or genetic disorders.
The obesogenic environment worsens this situation by limiting access to healthy and sustainable foods at affordable prices, lacking spaces for safe physical activity, and lacking appropriate policies to promote health. Furthermore, the lack of early detection by health systems exacerbates the problem.
Childhood and adolescent obesity not only affects their current health but is also associated with a higher risk of developing non-communicable diseases (NCDs), such as type 2 diabetes and cardiovascular diseases, at an early age.
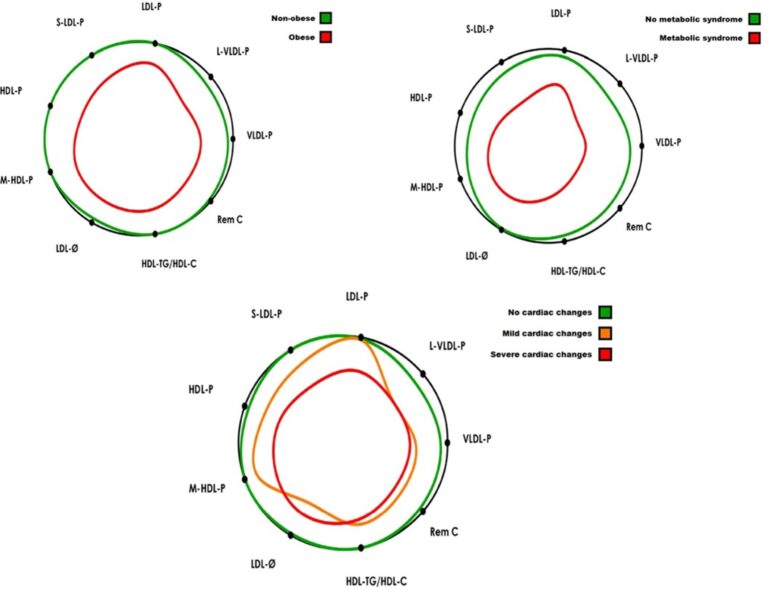
A recent study, led by Josep Manuel Siurana, Head of the Cardiology Department at HM Nens Hospital in Barcelona, and involving Anna Sabaté-Rotés, Núria Amigó, Neus Martínez-Micaelo, Larry Arciniegas, Lucia Riaza, Eduard Mogas, Ferran Rosés-Noguer, Paula S. Ventura, and Diego Yeste, examines how advanced lipoprotein profiles (obtained through nuclear magnetic resonance spectroscopy, NMR) are related to various degrees of cardiac impairment in adolescents with morbid obesity. The study evaluates the relationship between advanced lipoprotein testing (ALT), cardiac changes, metabolic syndrome (MS), and inflammatory markers in adolescents with a normal conventional lipid profile (CLP) and no type 2 diabetes.
It included 42 adolescents with morbid obesity and 25 with normal weight. The function and morphology of the left ventricle (LV) were evaluated using ALT, which measures lipoproteins through NMR. The results showed that adolescents with obesity had more atherogenic lipoprotein profiles, increasing their risk of developing cardiac abnormalities.
This study highlights the importance of using advanced analyses, such as the advanced Lipoprotein Test (Liposcale Test) from Biosfer Teslab, to identify adolescents with obesity who are at risk of developing cardiovascular diseases early, even when conventional test results appear normal.
Read the full article here and contact us.