Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma. While most patients respond favorably to initial treatment, a significant percentage develop relapsed or refractory (R/R) disease, which limits therapeutic options and worsens prognosis.
A recent study published in the journal Cancers has identified two metabolic biomarkers that may predict the clinical evolution of patients with R/R DLBCL. These are 3-hydroxybutyrate (3OHB) and acetone, compounds known as ketone bodies, whose presence in serum has been directly associated with survival in patients treated with a combination of lenalidomide, rituximab, gemcitabine, dexamethasone, and cisplatin (R2-GDP).
The study, conducted as part of the R2-GDP-GOTEL clinical trial, analyzed serum samples from 69 patients using nuclear magnetic resonance (NMR) spectroscopy. The results were significant:
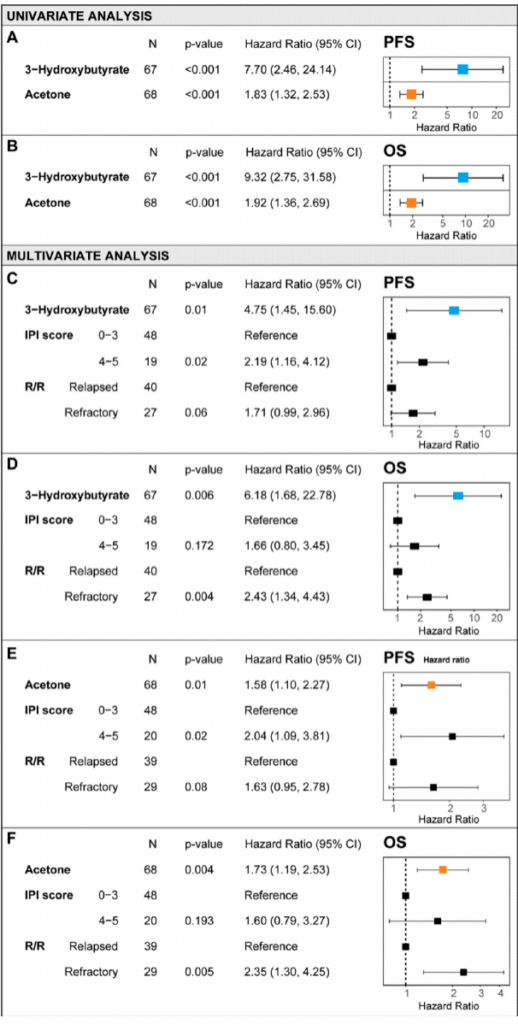
To facilitate the clinical application of these findings, the researchers designed predictive models, known as nomograms, that integrate 3OHB and acetone levels with other relevant clinical factors. These models demonstrated high predictive accuracy:
These results suggest that incorporating these biomarkers into patient evaluations could contribute to more personalized and precise therapeutic decision-making.
Cancer metabolism is an evolving field of research. It has been demonstrated that some tumor cells primarily rely on glycolysis for energy (Warburg Effect), while others utilize fatty acid oxidation and ketone bodies.
This study suggests that certain lymphomas, particularly those of the ABC subtype, may use ketone bodies as an energy source, which is associated with a poorer treatment response. The detection of elevated 3OHB and acetone levels in serum could indicate metabolic reprogramming of the tumor, allowing for the identification of patients with a worse prognosis and the adjustment of their therapeutic strategies accordingly.
While this study focused on patients treated with the R2-GDP regimen, further research is needed to:
This advancement represents a significant step toward precision oncology, where studying tumor metabolism could be key to predicting lymphoma progression and improving patient survival.
If you are a researcher and want to learn how NMR-based metabolomics can support your studies, do not hesitate to contact us! We would be delighted to explore new opportunities in biomarker analysis together and contribute to improving health through research.
Read the full article here.