Cardiovascular Disease: Beyond LDL Cholesterol
Cardiovascular disease (CVD) claims the lives of over 4 million people in Europe every year. Dyslipidemia, a disorder characterized by abnormal blood lipid levels, is one of the most significant risk factors for the development of CVD. Specifically, LDL cholesterol plays a central role in the relationship between cardiovascular disease and dyslipidemia. However, a high percentage of patients who meet therapeutic targets for LDL cholesterol, blood pressure, and glucose experience cardiovascular events.
One of the most relevant studies exemplifying the failure of LDL cholesterol as a risk marker for CVD is the study published in 2009 in the American Heart Journal, which included over 130,000 individuals hospitalized for acute coronary disease [1.] The study showed that over 50% of the patients had optimal levels of LDL cholesterol, one of the main risk factors for CVD [2,3].
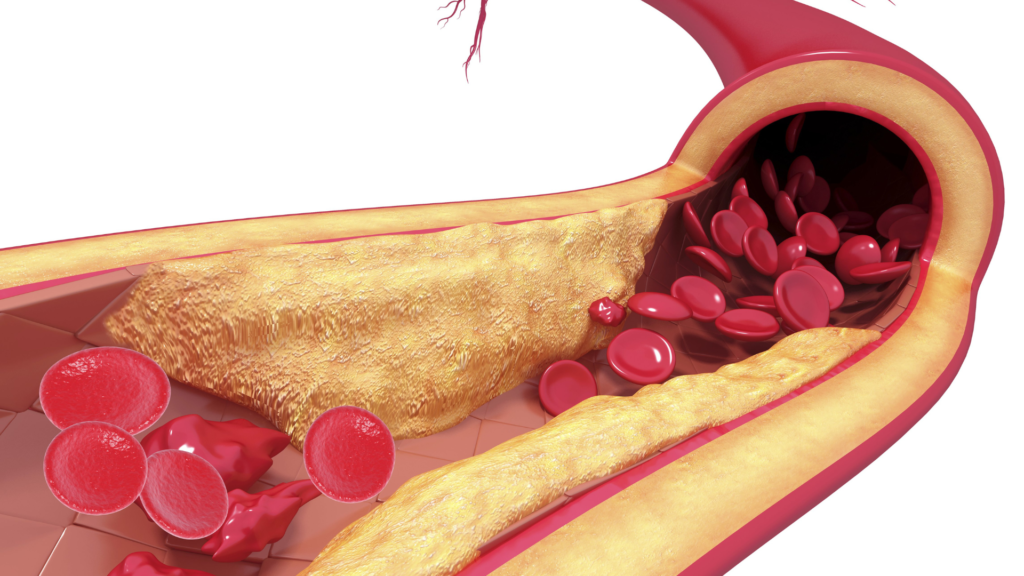
The excess of cardiovascular complications in patients with good LDL cholesterol control is defined as residual risk and is unacceptably high (60% – 70% relative risk). Among the possible causes of residual cardiovascular risk is atherogenic dyslipidemia (AD), a condition very common in individuals with metabolic disorders such as diabetes and obesity. AD is characterized by alterations in HDL and VLDL lipid classes, such as low HDL cholesterol levels and high triglycerides, but LDL cholesterol levels are usually normal or slightly elevated. However, the number of particles carrying it, p-LDL, is clearly increased due to the presence of smaller LDL particles, more capable of crossing arterial walls and accelerating the atherosclerotic process underlying CVD.

Regarding high-density lipoproteins (HDL), clinical studies suggest that the concentration of HDL particles (p-HDL) can provide information about an individual’s cardiovascular status that is independent of HDL cholesterol itself (c-HDL) [4,5]. In the MESA study, considering 5,598 men and women, c-HDL was not associated with CVD and intima-media thickness once adjusted for LDL cholesterol and p-LDL [6]. In contrast, p-HDL remained strongly and independently associated with CVD. Additionally, in the JUPITER study, Mora et al. indicated that the concentration of p-HDL under pharmacological treatment is a better marker of residual CVD risk than c-HDL concentration or apolipoprotein AI (ApoAI) concentration [7].
1: Sachdeva, A., Cannon, C. P., Deedwania, P. C., LaBresh, K. A., Smith Jr, S. C., Dai, D., … & Fonarow, G. C. (2009). Lipid levels in patients hospitalized with coronary artery disease: an analysis of 136,905 hospitalizations in Get With The Guidelines. American heart journal, 157(1), 111-117.
2: Otvos, J. D., Jeyarajah, E. J., & Cromwell, W. C. (2002). Measurement issues related to lipoprotein heterogeneity. The American journal of cardiology, 90(8), 22-29.
3: Kannel, W. B. (1995). Range of serum cholesterol values in the population developing coronary artery disease. The American journal of cardiology, 76(9), 69C-77C.
4: Qi, Y., Fan, J., Liu, J., Wang, W., Wang, M., Sun, J., … & Zhao, D. (2015). Cholesterol-overloaded HDL particles are independently associated with progression of carotid atherosclerosis in a cardiovascular disease-free population: a community-based cohort study. Journal of the American College of Cardiology, 65(4), 355-363.
5:deGoma, E. M., & Rader, D. J. (2012). High-density lipoprotein particle number: a better measure to quantify high-density lipoprotein?. Journal of the American College of Cardiology, 60(6), 517-520.
6: Mackey, R. H., Greenland, P., Goff, D. C., Lloyd-Jones, D., Sibley, C. T., & Mora, S. (2012). High-density lipoprotein cholesterol and particle concentrations, carotid atherosclerosis, and coronary events: MESA (multi-ethnic study of atherosclerosis). Journal of the American College of Cardiology, 60(6), 508-516.
7:Mora, S., Glynn, R. J., & Ridker, P. M. (2013). High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation, 128(11), 1189-1197.
8: Remaley, A. T. (2015). HDL cholesterol/HDL particle ratio: a new measure of HDL function?. Journal of the American College of Cardiology, 65(4), 364-366.
9: Qi, Y., Fan, J., Liu, J., Wang, W., Wang, M., Sun, J., … & Zhao, D. (2015). Cholesterol-overloaded HDL particles are independently associated with progression of carotid atherosclerosis in a cardiovascular disease-free population: a community-based cohort study. Journal of the American College of Cardiology, 65(4), 355-363


