Each year, cardiovascular diseases (CVD) are responsible for more than 4 million deaths in Europe, making them the leading cause of mortality on the continent. These diseases include heart attacks, strokes, and other conditions related to the circulatory system.
For decades, the prevention and treatment of CVD have focused on lowering LDL cholesterol (commonly known as “bad cholesterol”) since it has been identified as a key risk factor in atherosclerosis and artery blockage. However, recent studies have shown that controlling LDL cholesterol alone is not enough, as many patients who manage to lower their levels still develop cardiovascular diseases.
This has led to the need for a broader and more personalized approach to cardiovascular risk prevention, where other biomarkers and metabolic factors play a crucial role.
Residual risk refers to the percentage of patients who, despite achieving target levels of LDL cholesterol, blood pressure, and glucose, continue to suffer cardiovascular events. It is estimated that this risk is around 60-70%, indicating that other factors are still not being fully addressed in the prevention and treatment of CVD.
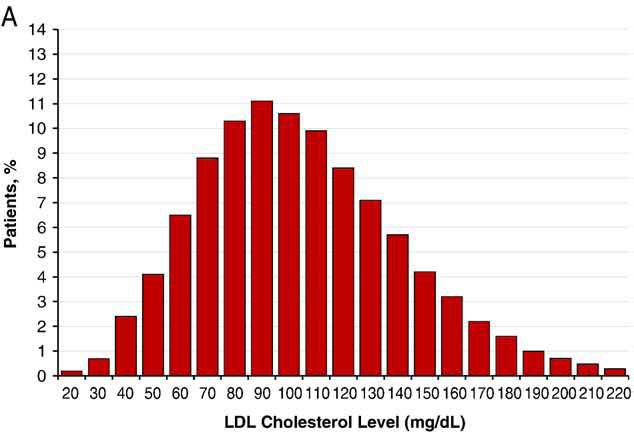
One of the most revealing studies in this area was published in the American Heart Journal in 2009. This study analyzed over 130,000 patients hospitalized for coronary artery disease and found that more than 50% of them had optimal LDL cholesterol levels at the time of admission. This suggests that LDL cholesterol alone is not a sufficient indicator of cardiovascular risk.
Cholesterol does not circulate freely in the blood; it requires a special transport system: lipoproteins. These particles, composed of lipids and proteins, are responsible for transporting cholesterol, triglycerides, and other lipids through the bloodstream to the cells that need them.
There are different types of lipoproteins, but the most relevant in cardiovascular health are:
Traditional blood tests measure total cholesterol, LDL, and HDL concentrations. However, these values do not accurately reflect the number and size of lipoproteins carrying that cholesterol, which can be crucial in assessing cardiovascular risk.
LDL Particle Number and Size: It is not just the total amount of LDL cholesterol that matters, but also the number of LDL particles transporting it. Smaller, denser particles can penetrate artery walls more easily, increasing the risk of atherosclerosis.
Atherogenic Dyslipidemia: A common lipid disorder in people with diabetes and obesity, characterized by low HDL cholesterol levels and excess triglycerides. Even if LDL cholesterol appears normal, the number of LDL particles is often high, increasing cardiovascular risk.
The Role of HDL Cholesterol: Traditionally, high HDL cholesterol levels were considered protective against CVD. However, recent studies indicate that it is not just the amount of HDL in the blood that matters but also its quality and functionality. Some HDL particles can lose their ability to remove cholesterol from arteries, becoming dysfunctional.
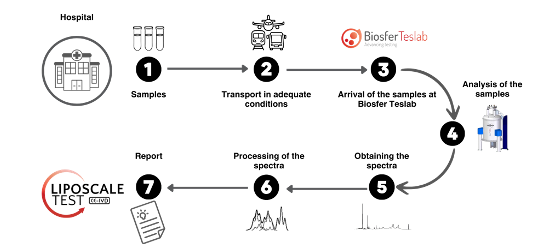
One of the most innovative tools in this field is Liposcale®, a test based on Nuclear Magnetic Resonance (NMR) that enables advanced characterization of the lipid profile, providing more detailed and accurate information than traditional cholesterol tests.
With this technology, it is possible to:
✅ Quantify the number and size of LDL, HDL, and VLDL particles, allowing for a more precise cardiovascular risk assessment beyond just measuring total cholesterol.
✅ Analyze the distribution of lipoprotein particles based on their size and concentration, helping to identify dyslipidemia subtypes that may go undetected with a conventional lipid profile.
✅ Evaluate the triglyceride fraction transported in each type of lipoprotein, which is crucial for studying atherogenic dyslipidemias and metabolic syndrome patients.
✅ Detect altered lipid profiles that might be overlooked in standard analyses, such as a high number of small, dense LDL particles, which are highly atherogenic.
✅ Offer a more personalized approach to cardiovascular prevention and treatment, allowing therapeutic strategies to be tailored to each patient based on their actual lipoprotein profile rather than just total cholesterol levels.
References:
Sachdeva, A., Cannon, C. P., Deedwania, P. C., et al. (2009). Lipid levels in patients hospitalized with coronary artery disease: an analysis of 136,905 hospitalizations in Get With The Guidelines. American Heart Journal, 157(1), 111-117. https://doi.org/10.1016/j.ahj.2008.08.010
Otvos, J. D., Jeyarajah, E. J., & Cromwell, W. C. (2002). Measurement issues related to lipoprotein heterogeneity. The American Journal of Cardiology, 90(8), 22-29. https://doi.org/10.1016/s0002-9149(02)02534-1
Mackey, R. H., Greenland, P., Goff, D. C., et al. (2012). High-density lipoprotein cholesterol and particle concentrations, carotid atherosclerosis, and coronary events: MESA (Multi-Ethnic Study of Atherosclerosis). Journal of the American College of Cardiology, 60(6), 508-516. https://doi.org/10.1016/j.jacc.2012.03.060
Mora, S., Glynn, R. J., & Ridker, P. M. (2013). High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation, 128(11), 1189-1197. https://doi.org/10.1161/CIRCULATIONAHA.113.002671
Qi, Y., Fan, J., Liu, J., et al. (2015). Cholesterol-overloaded HDL particles are independently associated with progression of carotid atherosclerosis in a cardiovascular disease-free population: a community-based cohort study. Journal of the American College of Cardiology, 65(4), 355-363. https://doi.org/10.1016/j.jacc.2014.11.041
Remaley, A. T. (2015). HDL cholesterol/HDL particle ratio: a new measure of HDL function? Journal of the American College of Cardiology, 65(4), 364-366. https://doi.org/10.1016/j.jacc.2014.11.044
Kannel, W. B. (1995). Range of serum cholesterol values in the population developing coronary artery disease. The American journal of cardiology, 76(9), 69C-77C.