Today, on International Familial Hypercholesterolemia (FH) Day, we want to highlight this genetic condition that affects millions of people worldwide and can lead to severe cardiovascular complications if not diagnosed and treated in time.

FH is a hereditary disorder characterized by extremely high levels of LDL cholesterol because the body does not properly eliminate cholesterol from the blood, causing its accumulation in the arteries. Since it is a genetic condition, early detection is crucial, ideally through family screening. However, it often goes unnoticed until damage to the cardiovascular system has already occurred.
A study published in “The Journal of Clinical Endocrinology & Metabolism” earlier this year, led by Dr. Daiana Ibarretxe from the Vascular and Metabolism Medicine Unit, Lipid and Atherosclerosis Research Unit at Sant Joan University Hospital, Rovira i Virgili University (URV), IISPV, titled “The Lipoprotein Profile Evaluated by 1H-NMR Improves the Performance of Genetic Testing in Familial Hypercholesterolemia,” emphasizes the importance of using NMR for better classification of FH patients. This optimizes genetic testing and allows for a more accurate stratification of cardiovascular risk.
One of the main challenges in treating familial hypercholesterolemia is correctly identifying patients with the monogenic form of the disease. Current genetic tests, while essential, do not always detect pathogenic variants. For example, studies in our region showed that only 41% of patients with high clinical scores on the DLCN index have a genetic variant, and surprisingly, 20% of patients with low clinical risk turned out to be genetically positive.
This discrepancy is partly due to the low accuracy of clinical indices and the difficulty in obtaining clear family histories. Additionally, many physical signs, such as corneal arcus or xanthomas, are less frequent due to the widespread use of statins. This underscores the need to improve diagnostic testing to reduce clinical errors and optimize treatment.
The study proposes an innovative solution: using nuclear magnetic resonance (1H-NMR) to deepen the analysis of the lipid profile, going beyond LDL cholesterol. Advanced tools like the Liposcale® test allow for the measurement not only of cholesterol concentration but also of the number, size, and composition of lipoprotein particles. This detailed analysis identified key metabolic patterns not seen in conventional tests, such as an increase in triglyceride-rich lipoproteins and more small HDL particles in genetically negative FH patients.
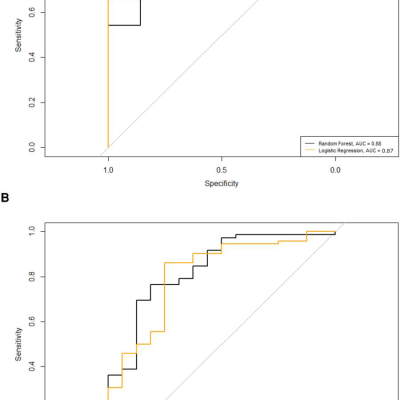
With this data, a formula was developed to classify patients more accurately, using parameters like the number of large LDL particles, HDL size, and remnant cholesterol. This formula has been shown to correctly classify 87% of adult patients and 82% of children with FH, significantly improving the performance of genetic tests.
Thanks to NMR metabolomics and tools like Liposcale®, we are moving towards personalized medicine that not only allows for earlier and more accurate diagnosis of FH but also facilitates the design of more effective treatments tailored to the individual characteristics of each patient. This is especially relevant in diseases like FH, where the risk of severe complications is high, and early intervention can make the difference between health and disease.
At Biosfer Teslab, we are committed to continuing the development and application of advanced technologies to improve the quality of life of people affected by FH and other metabolic diseases. If you want to learn more about our work or explore potential collaborations, do not hesitate to contact us.
Let’s work together for safer and more personalized cardiovascular health!